.

Does Cannabis Help To Treat Migraine Headaches?
Migraines land a much harder blow than regular headaches. They leave people nauseated, dizzy, and debilitated. Conventional medications work for many people, but others opt for a bowl full of green. Anecdotal data shows that many migraine sufferers find solace in the herb. Find out if cannabis might help to treat migraines in the future.
Contents:
- What are migraines?
- The link between migraines and cannabis
- What does the research say about cannabis and migraines?
- Can cannabis cause migraines?
- When and how to consume cannabis for migraines
- Cbd and migraines
- When and how to use cbd
- Migraines, the endocannabinoid system, and cannabis
- Which cannabis strains can help ease migraines and headaches?
The severity of migraines varies from one person to another. For some, they’re a mere annoyance, while others are left couchbound with visual disturbances, disorientation, and severe pain.
Many who suffer from the condition use nutrition and exercise as a preventative measure, and reach for strong painkillers and anti-sickness medicine when things get tough. However, some patients prefer to steer clear of conventional medicines, as they do little to alleviate the symptoms of resistant and refractory migraines[1].
As such, some individuals resort to smoking, vaping, and eating cannabis in an attempt to soothe themselves. Scores of anecdotes support this claim, and ongoing studies are investigating if and how the plant can help. So, does weed help with migraines? Read on to discover.
What Are Migraines?
A migraine is defined as a recurrent throbbing headache that typically affects one side of the head. They aren’t regular headaches; migraines tend to be much more severe and debilitating. The neurological condition also ranks as the most common headache disorder, with approximately 10% of the population experiencing a bout within a given year.
Unfortunately, most people don’t find much help in the medical system, as only one-third of patients receive proper treatment[2].
-
Symptoms of Migraine
Migraines are grouped into two categories: with aura, and without aura. Migraine auras are predominantly visual symptoms that set in before an attack, though they can occur during one as well. They often manifest as colored spots, blind spots, tunnel vision, and zig-zags. However, auras can also rear their head in the form of muscle weakness, confusion, pins and needles, and speech problems.
Regardless of whether auras are experienced, migraines share the following key symptoms in common:
| Headache attack lasting 4–72 hours | Pulsing/throbbing pain | Pain on one side of the head | Nausea and vomiting |
| Sensitivity to light and sound | Yawning | Irritability | Shoulder and neck stiffness |
| Headache attack lasting 4–72 hours | Pulsing/throbbing pain |
| Pain on one side of the head | Nausea and vomiting |
| Sensitivity to light and sound | Yawning |
| Irritability | Shoulder and neck stiffness |
-
What Causes Migraines?
The exact cause of migraines remains unknown, but researchers have developed several theories over the years in hopes of uncovering the roots of the pathology. Some of the most prominent include:
- Vascular theory: Until the mid-20th century, this theory posited that migraines strike when the carotid arteries (major blood vessels in the neck) become engorged[3].
- Neurovascular theory: This theory points toward the neurological origins of migraine, suggesting that the vascular changes are only secondary to happenings in the central nervous system[4].
- Neurotransmitter theory: Some research shows that migraine patients often produce low levels of serotonin; drugs that reduce the levels of this neurotransmitter increase the number of migraine attacks[5].
- Brain stem theory: This theory suggests that the periaqueductal gray matter region of the brainstem might generate migraine attacks[6].
- Biopsychosocial theory: Some researchers point toward the psychological elements of migraine, including influences of stress, pain catastrophising, and even personality[7].
Root causes aside, numerous factors can trigger a migraine attack, including:
| Emotional stress | Skipping a meal | Caffeine | Hormonal changes in females |
| Sensitivity to food preservatives | Changing weather conditions | Loud noises |
| Emotional stress | Skipping a meal | ||||||
| Caffeine | Hormonal changes in females | ||||||
| Sensitivity to food preservatives | Changing weather conditions | ||||||
| Loud noises | |||||||
|---|---|---|---|---|---|---|---|
The Link Between Migraines and Cannabis
So, where exactly does cannabis enter the picture? Why would a humble herb that sprouts from the ground have any positive effect on devastating migraine attacks? To answer that question, we need to take a peek into the endocannabinoid system, hereinafter referred to as the ECS.
Just as we possess a digestive system, nervous system, immune system, and musculoskeletal system, our bodies feature an ECS. All of these physiological systems fulfill unique functions; the immune system protects us from pathogens, and the digestive system helps us assimilate nutrients. And the ECS? This body-wide network is tasked with keeping other systems in balance. It maintains homeostasis—the biological sweet spot that keeps everything running smoothly. Not too fast, nor too slow.
The ECS comprises receptors, signalling molecules (known as endocannabinoids), and metabolic enzymes that synthesise and degrade endocannabinoids. A wide range of cell types create endocannabinoids on demand. These lipids then bind to ECS receptors to create the desired changes within target cells. Many different receptors make up the ECS, but cannabinoid receptor 1 (CB1) and cannabinoid receptor 2 (CB2) are the primary types.
This is where things get interesting. The cannabis plant produces molecules that are structurally similar to our endocannabinoids, known as phytocannabinoids. These chemicals are so similar to our own that they’re able to bind to ECS receptors and alter enzyme activity—we can essentially hack the ECS through the use of phytocannabinoids.
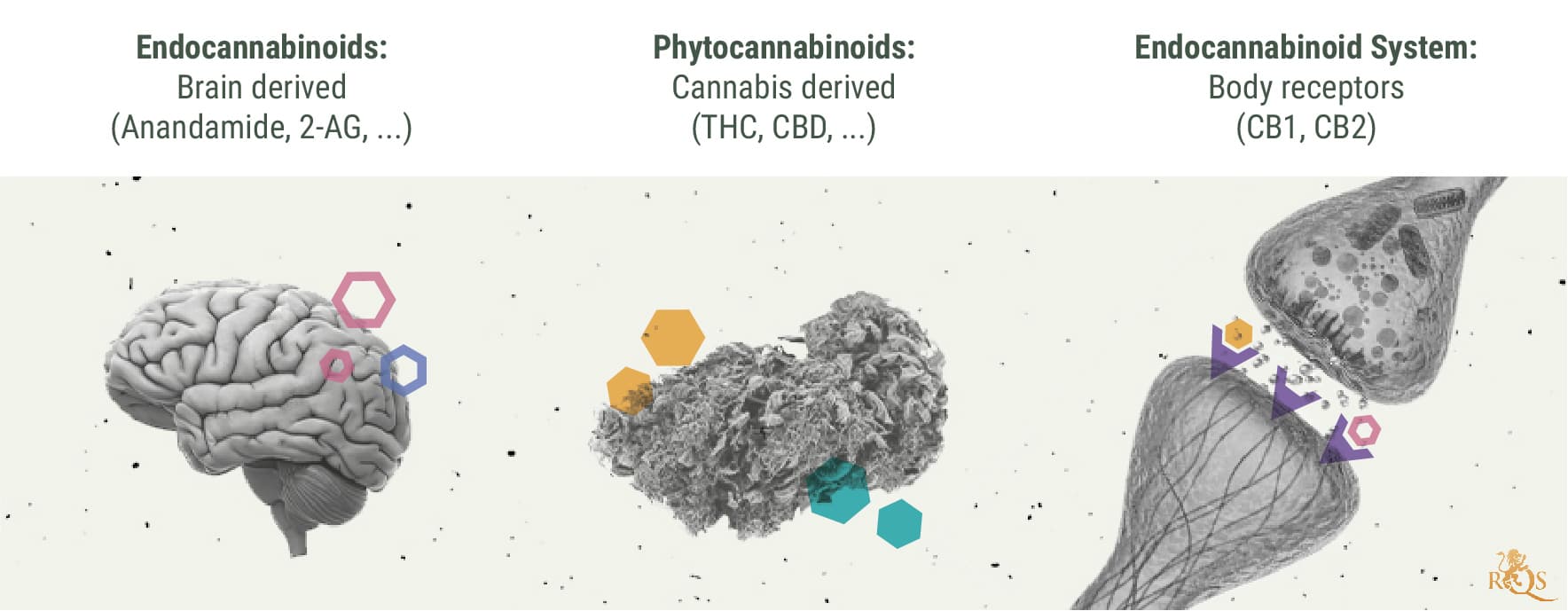
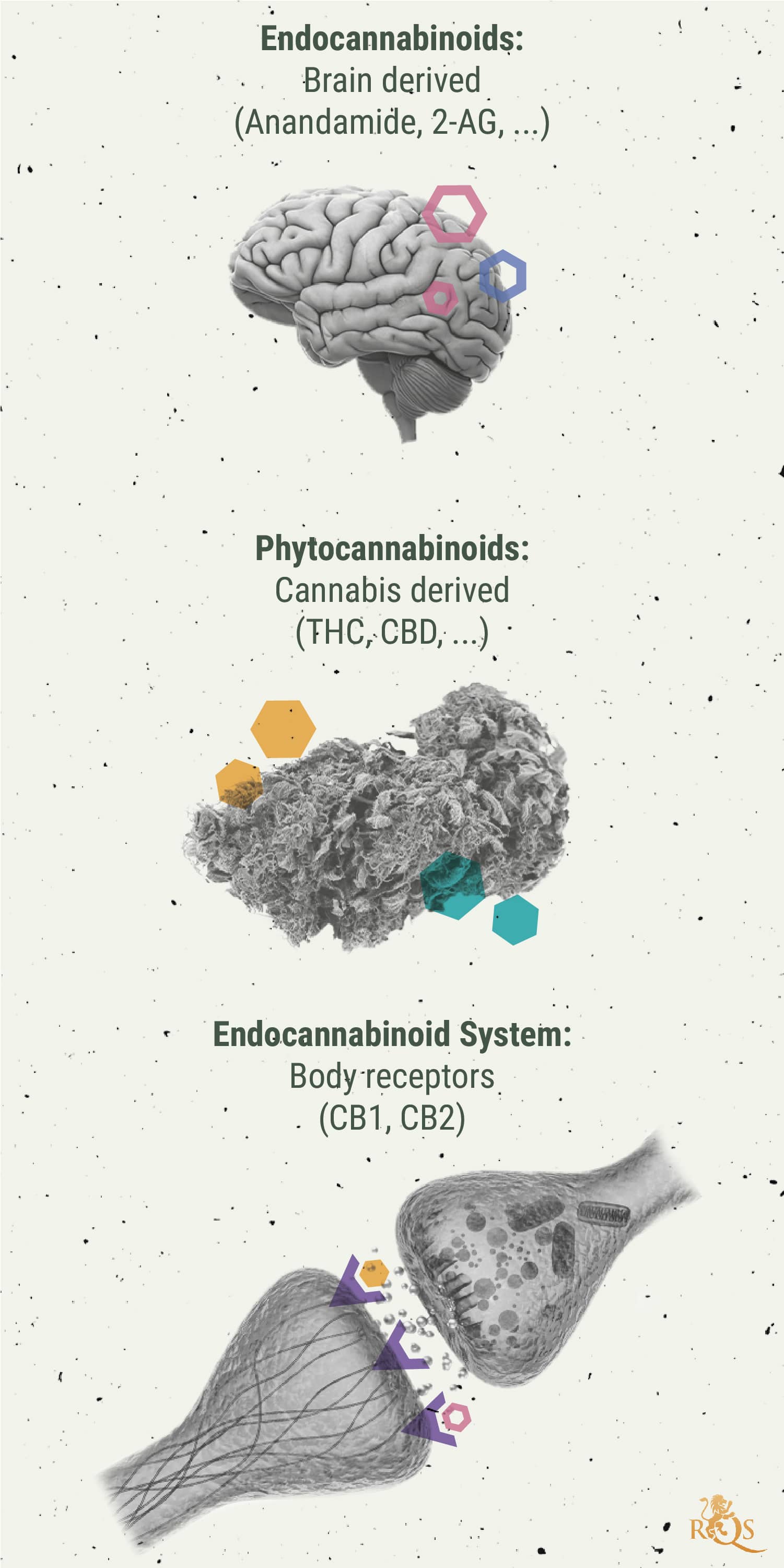
Because the ECS oversees other systems, it comes as no surprise that endocannabinoid levels are implicated in migraine attacks. Indeed, researchers have discovered a link between dysregulation of the ECS in the condition. Cells start to churn out the endocannabinoid anandamide in response to inflammation, a molecule that binds to both the CB1 and CB2 receptors. Clinical observations have identified reduced anandamide levels in cerebrospinal fluid and plasma samples taken from migraine patients[8].
In this regard, these findings place migraine alongside conditions such as fibromyalgia and irritable bowel syndrome. Lower levels of circulation endocannabinoids, or “low endocannabinoid tone”, is thought to potentially cause a dysregulation of the ECS known as clinical endocannabinoid deficiency[9]. Researchers are now exploring whether phytocannabinoids provide a worthy substitute to fulfill the role of their endogenous counterparts.
What Does the Research Say About Cannabis and Migraines?
These theories sound promising, but does cannabis help to alleviate migraine attacks in the real world? Plenty of people will tell you that puffing on a joint or hitting a bowl takes the edge off the throbbing pain and nausea. While encouraging, anecdotes don’t provide an accurate view of reality. Repeatable and vigorous scientific studies hold the answers to the efficacy of the herb. Unfortunately, controlled human trials currently don’t exist.
Below, we’ll delve into the available research to get as close to an answer as possible.
-
Medical Marijuana for Migraines
Does medical marijuana help migraines? It depends on what you mean by medical marijuana. These resinous flowers seem simple to the naked eye, but they contain hundreds of phytochemicals, including cannabinoids, terpenes, and flavonoids; all of these constituents have unique effects on the human body.
There are thousands of cultivars available, and each has a different ratio of these chemicals. As you can imagine, it’s hard to quantify exactly what’s happening at the cellular level. However, most ongoing studies are focused on high-THC medical marijuana varieties for migraine attacks.
A 2019 study conducted at Washington State University collected anecdotal data from over 1,300 migraine patients who used cannabis to treat their condition. An impressive 49.6% stated that the herb helped to reduce the severity of the attacks[10].
A 2021 study also collected anecdotal data using an online survey. They received answers from 589 adult cannabis users living in states where they had access to medical marijuana. Over 70% of the participants endorsed using cannabis to curb their migraine attacks. However, the researchers concluded that “future studies are needed to determine the cannabis forms, potencies, and dosages that are most effective at treating migraine headaches”[11].
A human trial titled “Efficacy of Inhaled Cannabis for Acute Migraine Treatment” is set for publication in December 2021. The phase two trial utilised both high-THC and high-CBD medical marijuana for migraines, and will add weight to existing anecdotal data[12].
Physiologically speaking, THC mimics anandamide at the CB1 receptor, yet to an even greater degree. In cases of clinical endocannabinoid deficiency, the psychotropic cannabinoid could theoretically fill in for anandamide and temporarily fulfill its function.


-
Dronabinol and Migraines
A synthetic version of THC, dronabinol was approved in 1985 by the Food and Drug Administration (FDA) for the treatment of chemotherapy-induced nausea and vomiting. Ongoing research is determining the efficacy of the medication in the treatment of chronic migraine headaches and refractory cluster headaches[14].
Dronabinol binds with the same receptor sites as THC. However, patients can only access the medicine as oral capsules. This method of administration converts the molecule into the more potent 11-hydroxy-THC in the liver, leading to intoxicating effects that some patients find unpleasant. The FDA has yet to approve dronabinol for the treatment of migraine. Moreover, their prescribing information document lists headaches as an adverse effect of the medication[15].
Can Cannabis Cause Migraines?
Even if cannabis works for someone suffering from migraines, they might find their attacks returning with a vengeance. Some patients experience a new kind of headache, or a significantly worse version of their original malady, when using cannabis too frequently. Known as rebound headaches or medication-overuse headaches, this phenomenon can occur with several different types of medication.
However, the research remains early and unclear in the case of cannabis. A preliminary study conducted at Stanford University School of Medicine found that patients with chronic migraines who use cannabis are around six times more likely to experience overuse headaches than those who don’t. However, the researchers are still unsure of the association between the two, and if patients are simply using cannabis to treat rebound headaches, as opposed to the herb directly causing the condition[16].
When and How To Consume Cannabis for Migraines
There are multiple options to consider when it comes to using cannabis for migraine attacks. Most of the research focuses on inhaled cannabis, but some people prefer to chow down on edibles.
| Smoking | Smoking weed delivers cannabinoids almost directly into the bloodstream via the alveoli of the lungs. This route of administration results in near-instant effects. But smoking comes with obvious downsides, especially when using tobacco alongside weed to craft spliffs. As well as damaging lung health, smoking can trigger headaches in some people. |
| Vaping | Vaping also delivers a rapid hit of cannabinoids, although this method uses lower temperatures than smoking. Instead of combusting cannabis flowers, vaporizers use conduction or convection heating systems to vaporize cannabinoids and terpenes, resulting in less tar and toxic chemicals. Studies exploring vaping for migraines also found no association between the route of administration and overuse headaches.[10] |
| Edibles | Edibles offer a different route of administration to inhaled cannabis. Eating infused treats sends THC through the stomach and liver, converting the molecule into 11-hydroxy-THC. While some users aren’t keen on the potency of the experience, others revel in the borderline-psychedelic effects. This option might work for some users, but it’s best reserved for the evenings, away from work and other responsibilities. |
| Smoking | Smoking weed delivers cannabinoids almost directly into the bloodstream via the alveoli of the lungs. This route of administration results in near-instant effects. But smoking comes with obvious downsides, especially when using tobacco alongside weed to craft spliffs. As well as damaging lung health, smoking can trigger headaches in some people. |
| Vaping | Vaping also delivers a rapid hit of cannabinoids, although this method uses lower temperatures than smoking. Instead of combusting cannabis flowers, vaporizers use conduction or convection heating systems to vaporize cannabinoids and terpenes, resulting in less tar and toxic chemicals. Studies exploring vaping for migraines also found no association between the route of administration and overuse headaches.[10] |
| Edibles | Edibles offer a different route of administration to inhaled cannabis. Eating infused treats sends THC through the stomach and liver, converting the molecule into 11-hydroxy-THC. While some users aren’t keen on the potency of the experience, others revel in the borderline-psychedelic effects. This option might work for some users, but it’s best reserved for the evenings, away from work and other responsibilities. |
CBD and Migraines
CBD is a major constituent of cannabis, and plenty of research has looked into its clinical potential. Unfortunately, no scientific studies have specifically examined how CBD affects migraines. The limited research available on cannabis and headaches has tested both CBD and THC simultaneously, and, while producing some positive results, does not offer accurate insight into how CBD alone might affect headache or migraine sufferers.
While the jury is out on how exactly CBD may impact migraine and its symptoms, anecdotal evidence is mounting. In 2021, Utah-based CBD company Axon Relief published a survey[16] asking its customers to rate how Axon CBD products (which are all specially formulated to provide migraine relief) affected their headaches and migraines.
The survey asked 105 participants to rate their migraines using the Headache Impact Test (Hit-6™), a scientifically validated measure for headache and migraine intensity. It found that after 30 days of using Axon products, 86% of respondents noted a decrease in their headaches/migraines. On average, the participants experienced close to four fewer headache days than usual. Those participants regarded as chronic migraine sufferers (people who experience 15 to 29 headache days over a 30-day period) noted a 33% reduction in their headaches.
While we're still lacking specific research into CBD in this domain, studies have shown that the endocannabinoid system in general could be a great target for migraine treatments. The CB1 receptor is extremely abundant throughout the brain, and studies have shown that its activation (either by endo or phyto-cannabinoids) can affect many neurological pathways related to pain[17].
Now, CBD doesn't naturally have a high affinity for CB1 receptors. However, studies suggest[18] that it might act on over 65 different molecular targets in much more complex ways. And while many of these targets might lie outside of what is generally considered the ECS, it still acts on receptors that could play a potential role in the treatment of headaches or migraines. These include:
- 5-HT1A serotonin receptors
- TRPV1: Also known as "capsaicin receptors", TRPV1 receptors can be activated by eugenol, an essential oil in vanilla bean, which has a long history[19] of use for headaches, particularly among ancient Egyptian civilisations.
- GPR55[20]
Are There Risks to Taking CBD for Migraines?
In late 2017[21], the World Health Organization concluded that CBD in its pure state does not appear to have abuse potential or to cause harm. However, CBD isn't without side effects[22]; it can cause nausea, fatigue, and irritability in some people, and it can also compete for liver enzymes during metabolism, possibly affecting the rate at which the body breaks down many medications.
Moreover,recent research[23] claims that using cannabis while experiencing headaches and migraines may cause people to experience "rebound headaches". The study explains that this is typically caused by an "overuse" of cannabis and the fact that smoking or vaping can dry out mucous membranes.
When and How to Use CBD
When it comes to dealing with migraines, it is best to avoid smoking. As we mentioned above, smoking CBD, cannabis, or any other herb for that matter, dries out mucous membranes and increases the thickness of saliva—something you want to avoid when you're already suffering from a headache.
At the same time, seeing that migraines and headaches can set in extremely quickly, many people opt for CBD administration methods with a high bioavailability and a faster onset of effects.
Below are some of the most common ways in which migraine and headache sufferers use CBD:
| CBD oils and tinctures | CBD oils and tinctures can be taken sublingually, where they are partially absorbed via the mucous membranes of the mouth and have a faster onset of roughly 15 minutes. |
| CBD oral spray |
Oral CBD sprays are designed to be absorbed in the mouth rather than digested, and thereby can take effect in up to 15 minutes—similar to sublingually administered CBD oils. |
| Vaped CBD flower or concentrate | Vaping CBD boasts the fastest onset time, delivering effects in a matter of minutes. However, like smoking, vaping CBD may dry out mucous membranes. Plus, dosing vaped CBD (especially dry flower) is much less accurate than dosing CBD drops or an oral spray, putting you at a potentially higher risk of experiencing a rebound headache. If you must vape CBD to treat a headache or migraine, remember to stay well-hydrated and carefully watch your dose. |
| CBD oils and tinctures | CBD oils and tinctures can be taken sublingually, where they are partially absorbed via the mucous membranes of the mouth and have a faster onset of roughly 15 minutes. |
| CBD oral sprays |
Oral CBD sprays are designed to be absorbed in the mouth rather than digested, and thereby can take effect in up to 15 minutes—similar to sublingually administered CBD oils. |
| Vaped CBD flower or concentrate |
Vaping CBD boasts the fastest onset time, delivering effects in a matter of minutes. However, like smoking, vaping CBD may dry out mucous membranes. Plus, dosing vaped CBD (especially dry flower) is much less accurate than dosing CBD drops or an oral spray, putting you at a potentially higher risk of experiencing a rebound headache. If you must vape CBD to treat a headache or migraine, remember to stay well-hydrated and carefully watch your dose. |


Migraines, the Endocannabinoid System, and Cannabis
The bottom line: we need clinical trials to clear the murky waters and demonstrate the efficacy of cannabis for migraine attacks. However, the anecdotal evidence paints a promising picture. On top of this, research into clinical endocannabinoid deficiency hints that the ECS might underpin the pathophysiology of the condition.
Which Cannabis Strains Can Help Ease Migraines and Headaches?
Some cannabis strains appear to work better for people experiencing migraine attacks than others. Based on anecdotal feedback from users, these cultivars stand out above the rest in our extensive genetic archive. Buckle up for high levels of THC, mouth-watering terpene profiles, and rewarding yields.
White Widow
White Widow, named for her beautiful white coat of sparkling trichomes, is one of the most legendary cannabis strains around the world. Many consider this balanced 50/50 indica/sativa hybrid to be one of the best and most consistent cultivars to grow and smoke. She delivers a phenomenally powerful, almost psychedelic high that is cerebral but also incredibly relaxing. Her flavor is fresh and clean, with notes of pine and hints of citrus. With 19% THC, White Widow can be a good choice to soothe an oncoming migraine.
White Widow
|
|
White Widow S1 |
|
|
16 to 19 oz/m² |
|
|
2 to 3 feet |
|
|
8 - 10 weeks |
|
|
THC: 19% |
|
|
Sativa 50% Indica 50% |
|
|
19 to 21 oz/plant |
|
|
5 to 6 feet |
|
|
Early October |
|
|
Powerful , Stoned |
OG Kush
OG Kush is a classic strain that’s still a favorite among many cannabis users. Devout fans love the strain for its very intense smoke with the typical OG dankness and slight citrus kick. But of everything, what people love most about this 75% indica is her immense potency. Her effect is extremely relaxing on the body and the mind. This makes the iconic West Coast strain also a favorite among medicinal users looking to banish the varied physiological symptoms of migraines.
OG Kush
|
|
Chemdawg x Lemon Thai x Pakistani Kush |
|
|
15 to 17 oz/m² |
|
|
3 to 5 feet |
|
|
7 - 9 weeks |
|
|
THC: 19% |
|
|
Sativa 25% Indica 75% |
|
|
18 to 19 oz/plant |
|
|
6 to 7 feet |
|
|
October |
|
|
Calming, Uplifting |
Chocolate Haze
The popular Chocolate Haze is an almost pure (95%) sativa that’s perfect for all those who suffer from conditions such as arthritis, muscle pain, stress, and migraines. Her effect is extremely powerful yet pleasantly uplifting and cerebral. Her sunny and upbeat high make Chocolate Haze also a good choice for those looking to boost their mood. She will spoil you with her characteristic chocolate taste that blends with sweet and earthy notes.
Chocolate Haze
|
|
OG Chocolate Thai x Cannalope Haze |
|
|
17 to 18 oz/m² |
|
|
3 to 5 feet |
|
|
9 - 11 weeks |
|
|
THC: 20% |
|
|
Sativa 95% Indica 5% |
|
|
16 to 18 oz/plant |
|
|
5 to 7 feet |
|
|
Late October |
|
|
Heavy |
Sour Diesel
Sour Diesel is one of the most famous strains, and not just for her unique flavor that many cannabis enthusiasts love. Hailing from sunny California, this predominantly sativa hybrid delivers an awesomely potent and very aromatic smoke where she blends trademark fuel notes with herbal and sour flavors. With 19% THC, she delivers a powerful body high that is excellent for soothing headaches and easing stress.
Sour Diesel
|
|
Original Diesel x (Northern light x Shiva x Hawaiian) |
|
|
17 to 18 oz/m² |
|
|
3 to 5 feet |
|
|
10 - 11 weeks |
|
|
THC: 19% |
|
|
Sativa 70% Indica 30% |
|
|
19 to 21 oz/plant |
|
|
5 to 7 feet |
|
|
Late October |
|
|
Clear, Physically Relaxing |
Green Crack Punch
Green Crack Punch is a truly special cannabis strain. A mix of Green Crack, a strain known for her uplifting and energetic effect, and Purple Punch, massively potent in its own right, Green Crack Punch is a very relaxing indica heavy-hitter. The combo of these two strains makes for an awesome effect. You will feel motivated and energised while she will relax your body from head to toe. With her powerful effect (she measures up to 20% THC), this 60% indica is an ideal choice for medicinal users who want a flexible strain to dose throughout the day.
Green Crack Punch
|
|
Green Crack x Purple Punch |
|
|
16 to 19 oz/m² |
|
|
3 to 5 feet |
|
|
8 - 9 weeks |
|
|
THC: 18% |
|
|
Sativa 60% Indica 40% |
|
|
19 to 21 oz/plant |
|
|
6 to 7 feet |
|
|
Late September |
|
|
Calming, Euphoric |
Medical DisclaimerInformation listed, referenced or linked to on this website is for general educational purposes only and does not provide professional medical or legal advice.
Royal Queen Seeds does not condone, advocate or promote licit or illicit drug use. Royal Queen Seeds Cannot be held responsible for material from references on our pages or on pages to which we provide links, which condone, advocate or promote licit or illicit drug use or illegal activities. Please consult your Doctor/Health care Practitioner before using any products/methods listed, referenced or linked to on this website.
- European headache federation consensus on the definition of resistant and refractory migraine | The Journal of Headache and Pain | Full Text https://thejournalofheadacheandpain.biomedcentral.com
- https://www.sciencedirect.com/science/article/pii/S1875459712000379
- PERSONALITY FEATURES AND REACTIONS OF SUBJECTS WITH MIGRAINE | Archives of Neurology & Psychiatry | JAMA Network https://jamanetwork.com
- Migraine pathogenesis: the neural hypothesis reexamined. | Journal of Neurology, Neurosurgery & Psychiatry https://jnnp.bmj.com
- https://headachejournal.onlinelibrary.wiley.com/doi/10.1111/j.1526-4610.2012.02168.x
- https://headachejournal.onlinelibrary.wiley.com/doi/full/10.1046/j.1526-4610.2001.041007629.x
- OBM Neurobiology | Psychological Considerations in the Etiology and Pathophysiology of Migraines https://www.lidsen.com
- https://www.researchgate.net/publication/323849698_Endocannabinoid_System_and_Migraine_Pain_An_Update
- Clinical Endocannabinoid Deficiency Reconsidered: Current Research Supports the Theory in Migraine, Fibromyalgia, Irritable Bowel, and Other Treatment-Resistant Syndromes - PMC https://www.ncbi.nlm.nih.gov
- DEFINE_ME https://www.jpain.org
- https://www.sciencedirect.com/science/article/pii/S0965229920318860
- Efficacy of Inhaled Cannabis for Acute Migraine Treatment - Full Text View - ClinicalTrials.gov https://clinicaltrials.gov
- FAAH inhibition as a preventive treatment for migraine: A pre-clinical study - PubMed https://pubmed.ncbi.nlm.nih.gov
- The Use of Cannabis for Headache Disorders - PMC https://www.ncbi.nlm.nih.gov
- https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018651s029lbl.pdf
- Medication Overuse Headache in Chronic Migraine Patients Using Cannabis: A Case-Referent Study | Research Square https://www.researchsquare.com
- Study Finds CBD Is An Effective Treatment For Migraine https://www.forbes.com
- Cureus | Cannabinoid Receptors and Their Relationship With Chronic Pain: A Narrative Review https://www.cureus.com
- Molecular Targets of Cannabidiol in Neurological Disorders - PMC https://www.ncbi.nlm.nih.gov
- Targeting Serotonin1A Receptors for Treating Chronic Pain and Depression - PMC https://www.ncbi.nlm.nih.gov
- Use vanilla and other natural remedies to relieve and prevent headaches - NaturalNews.com https://www.naturalnews.com
- GPR55 in the brain and chronic neuropathic pain - PubMed https://pubmed.ncbi.nlm.nih.gov
- Drugs (psychoactive): Cannabidiol (compound of cannabis) https://www.who.int
- Cannabidiol (CBD): What we know and what we don't - Harvard Health https://www.health.harvard.edu
- Cannabis Use Linked to Increased Prevalence of MOH Among Chronic Migraineurs https://www.ajmc.com